What is Posttraumatic Stress Disorder?
Understanding the Condition, Its Symptoms, Risk Factors, and Treatment Options
Alex Penrod, MS, LPC, LCDC — Founder & EMDR Therapist | Neuro Nuance Therapy and EMDR, PLLC | Austin, TX
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after an individual experiences or witnesses a traumatic event. It was first recognized as "shell shock" in war Veterans, but has since been recognized as a condition that can develop in anyone exposed to severe and life-threatening events. PTSD can have a profound impact on an individual's daily life, everyday activities, relationships, and overall functioning, impacting physical health and leading to mental health problems. This page provide an overview of the condition as well as evidence based treatments.
PTSD Quick Facts
- 6–8% of adults experience PTSD at some point in their lives.
- Women are twice as likely as men to develop PTSD.
- 44% recover naturally within about three years; recovery without treatment becomes less likely over time.
- EMDR therapy achieves remission in roughly 36–90% of cases across studies.
- Recognized as a first-line treatment by the VA/DoD and NICE clinical guidelines.
- Long-term follow-ups show durable results at 6–12 months post-treatment.
Definition of PTSD
PTSD is characterized by intense, distressing thoughts, emotions, and reactions related to a traumatic experience that don’t resolve on their own. A traumatic event can include military combat, physical assault, physical abuse, sexual abuse, natural disasters, car accidents, domestic violence, or other life-threatening highly stressful events. People with PTSD may involuntarily relive the traumatic event through flashbacks, upsetting memories, or nightmares, avoid reminders of the trauma, experience negative thoughts, beliefs, and moods, and have a hard time managing heightened nervous system arousal.
These symptoms may occur briefly in Acute Stress Disorder immediately following a traumatic event, but if they continue for more than 30 days a person may be developing PTSD. People can experience some of the clinical features of PTSD in response to less severe non-life-threatening events, but this may fall into the category of an adjustment disorder.
The defining features of PTSD are exposure to a traumatic event and the specific symptoms of post-traumatic stress disorder occurring for more than 30 days.
Symptoms of PTSD
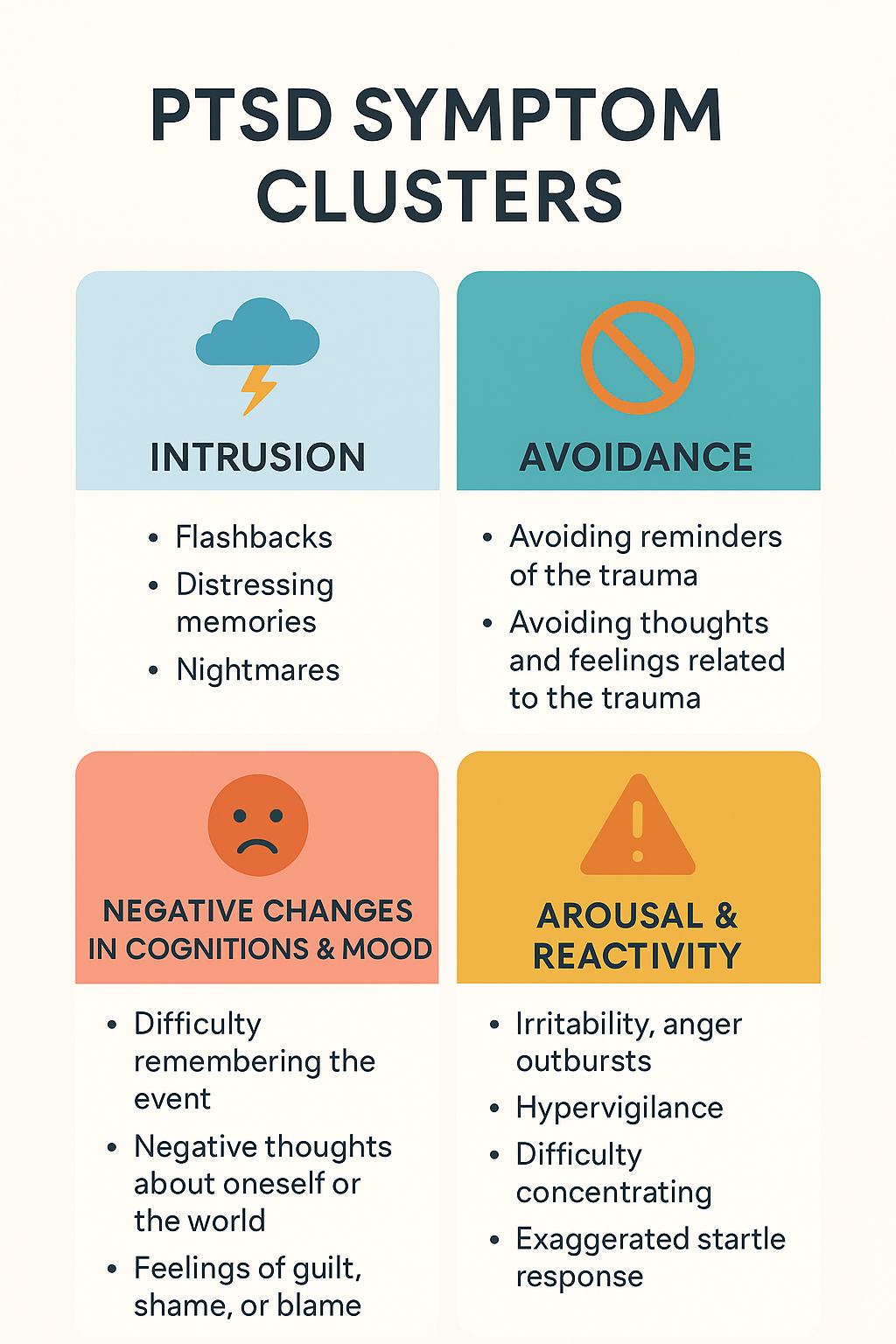
Post-traumatic stress disorder symptoms are typically grouped into four main categories:
Intrusive Thoughts
These include recurrent, involuntary memories, flashbacks, or distressing dreams related to the traumatic event. In severe cases, flashbacks may feel so vivid that the person feels as if they are reliving the event.
Avoidance Symptoms
Individuals with PTSD often go to great lengths to avoid reminders of the traumatic event. This could involve behavioral symptoms like avoiding certain places, people, activities, or even thoughts and feelings associated with the trauma.
Negative Changes in Mood and Thoughts
This includes symptoms like feelings of guilt, shame, fear, or hopelessness. Sometimes even positive emotions are difficult to tolerate.
Individuals may experience distorted beliefs about themselves or others, such as believing they are to blame for the trauma or that the world is entirely unsafe.
They may also have difficulty recalling important memories of the event.
Hyperarousal and Reactivity
People with PTSD may feel constantly "on edge," with increased heart rate, and easily startled.
Symptoms can include irritability, angry outbursts, reckless behavior, difficulty sleeping, and problems with concentration.
Diagnostic Criteria for PTSD
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Text Revision (DSM-5-TR), a diagnosis of PTSD is made by a mental health professional based on the following criteria:
Exposure to Trauma
The person must have been exposed to actual or threatened death, serious injury, or sexual violence.
This exposure can be direct, witnessed, or indirectly experienced through close friends or family members.
Presence of Intrusion Symptoms
At least one intrusive re-experiencing symptom (e.g., flashbacks, nightmares, intrusive memories) related to the trauma must be present.
Avoidance
At least one symptom of avoidance must be present, such as avoiding distressing memories, thoughts, feelings, or external reminders of the trauma.
Negative Alterations in Cognition and Mood
At least two symptoms, such as persistent negative emotional states, distorted beliefs, or detachment from others, must be present.
Marked Alterations in Arousal and Reactivity
At least two symptoms related to hyperarousal, such as irritability, hypervigilance, or an exaggerated startle response, must be present.
Duration
Symptoms must persist for more than one month.
Significant Distress or Impairment
The symptoms must cause significant distress or impairment in social, occupational, or other important areas of functioning.
Not Attributable to Substance Use or Medical Conditions
The symptoms must not be the result of substance use, medication, or other medical conditions.
Prevalence of PTSD Among Various Populations
PTSD can affect anyone who has experienced a traumatic event, but certain populations are more at risk:
General Population
In the general population, the lifetime prevalence of PTSD is estimated to be around 6-7%.
Women are twice as likely to develop PTSD as men, potentially due to a higher risk of exposure to certain types of trauma, such as sexual assault.
Military Veterans
Among U.S. Veterans, rates of PTSD vary by era and deployment history.
Approximately 7% of all Veterans experience PTSD in their lifetime.
In combat-exposed cohorts such as Vietnam and post-9/11 Veterans, prevalence can range from 10-30%
First Responders
Police officers, firefighters, paramedics, and other first responders are frequently exposed to traumatic events in the line of duty, which increases their risk for PTSD.
A recent systematic review and meta-analysis of global prevalence of PTSD among all first responder types showed around 14% of workers with routine trauma exposure developed PTSD.
A recent scoping review found a 57% prevalence rate of PTSD for firefighters, making this an especially high risk sub-group.
A recent systematic review and meta-analysis of pooled data from paramedics showed a 12-month prevalence rate of 20% for PTSD.
Survivors of Sexual Assault and Domestic Violence
Survivors of sexual assault, childhood abuse, or domestic violence have a high risk of developing PTSD.
A meta-analysis of studies indicated that up to 75% of sexual assault survivors meet criteria for PTSD in the first month after an assault with up to 41% still meeting criteria after a year.
Refugees and Asylum Seekers
Individuals fleeing war, persecution, or violence are at high risk for PTSD due to repeated trauma and ongoing stressors.
The prevalence of PTSD in refugee populations is estimated to be as high as 30% in general and up to 50% in some African populations.
Risk Factors for Developing PTSD
Several factors can increase an individual's risk of developing PTSD after a traumatic event. These risk factors can be categorized into pre-traumatic, peri-traumatic, and post-traumatic factors:
Pre-Traumatic Risk Factors
Personal or Family History of Mental Illness
A history of anxiety, depression, or other mental health disorders can increase the risk of developing PTSD.
Childhood Trauma
Individuals who have experienced trauma during childhood, such as abuse or neglect, are more likely to develop PTSD after a traumatic event in adulthood.
Personality Traits
Certain personality traits, such as a tendency towards neuroticism or a lack of resilience, can increase susceptibility to PTSD.
Lack of Social Support
A limited social support network or poor relationships with family and friends can elevate the risk of PTSD following a trauma.
Gender
Women are generally at a higher risk of developing PTSD, potentially due to a higher likelihood of experiencing trauma like sexual assault.
Peri-Traumatic Risk Factors
Severity of Trauma
The more severe or life-threatening the traumatic event, the higher the likelihood of developing PTSD.
Perceived Threat to Life
If an individual perceives their life to be in imminent danger during the traumatic event, the risk of PTSD is increased.
Dissociation During Trauma
Experiencing dissociation (feeling detached from reality) during a traumatic event is associated with a higher risk of developing PTSD.
Post-Traumatic Risk Factors
Lack of Access to Support Services
Limited access to psychological support, counseling, or other mental health services can increase the risk of PTSD.
Ongoing Stress or Exposure to Trauma
Continued exposure to stress or additional traumatic events can exacerbate PTSD symptoms.
Negative Coping Strategies
Harmful coping mechanisms, such as substance abuse, avoidance behaviors, and self-destructive behavior, can increase PTSD risk.
Protective Factors Against PTSD
While several risk factors can increase the likelihood of developing PTSD, certain protective factors can help reduce the risk or severity of PTSD symptoms:
Strong Social Support
A supportive network of friends, family, or community members can help buffer against PTSD by providing emotional support, validation, and a sense of belonging.
Family therapy can be important for learning how to support a loved one with PTSD.
Effective Coping Strategies
Positive coping mechanisms, such as problem-solving, emotional regulation, mindfulness, and seeking support, can reduce the impact of trauma and lower PTSD risk.
Resilience
Resilience is the ability to adapt well in the face of adversity, trauma, or stress. Individuals with higher levels of resilience are less likely to develop PTSD.
Access to Mental Health Care
Timely access to mental health care, including therapy and counseling, can prevent PTSD from developing or reduce its severity.
Psychoeducation
Understanding PTSD, its symptoms, and its treatments can empower individuals to seek help and engage in their recovery process.
Common Co-Occurring Disorders with PTSD
PTSD often coexists with other psychiatric disorders and mental health conditions like depression and anxiety, which can complicate diagnosis and treatment:
Depression
Major depressive disorder (MDD) is one of the most common co-occurring disorders with PTSD.
It’s characterized by persistent feelings of sadness, hopelessness, and loss of interest in previously enjoyed activities.
Up to 50% of individuals with PTSD may also experience MDD.
When depression leads to suicidal thoughts, it's vital to seek crisis services such as the Crisis Lifeline (dial 988) and follow-up with treatment.
Anxiety Disorders
Generalized anxiety disorder (GAD), panic disorder, social anxiety disorder, and other anxiety disorders frequently co-occur with PTSD.
The heightened state of fear and hypervigilance in PTSD can exacerbate anxiety symptoms.
The presence of an anxiety disorder prior to a traumatic event can be a risk factor for developing PTSD.
Substance Use Disorders
Individuals with PTSD may turn to drug or alcohol use as a way to cope with or self-medicate their symptoms, leading to substance use disorders.
Estimates suggest that up to 40-50% of people with PTSD also struggle with substance use.
Dissociative Disorders
Dissociative symptoms, such as depersonalization or dissociative amnesia, are common in PTSD, especially in cases involving complex trauma or repeated trauma.
Dissociative identity disorder (DID) may also co-occur in more severe cases involving child abuse and complex PTSD.
Evidence-Based Treatments for PTSD
There are several evidence-based and effective treatments for PTSD endorsed by organizations such as the American Psychiatric Association. These include trauma-focused psychotherapies and medications with strong evidence from randomized controlled trials. Trauma-focused psychotherapy is distinct from general talk therapy in that it’s aimed at desensitizing traumatic memories to reduce PTSD symptoms. The choice of treatment depends on the individual's symptoms, co-occurring disorders, and personal preferences.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a therapy that involves recalling distressing memories while engaging in bilateral stimulation (eye movement, alternating tones, or tapping).
This process helps reprocess traumatic memories and reduce their emotional charge.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
TF-CBT is a structured, short-term treatment that focuses on helping individuals process and reframe their traumatic memories.
It involves techniques such as cognitive restructuring, exposure therapy, and stress management.
Prolonged Exposure Therapy (PE)
Prolonged exposure therapy involves repeatedly talking through the trauma narrative in a safe and controlled environment.
This process helps individuals confront their fears, desensitize memories, and reduce avoidance behaviors, leading to symptom reduction.
Cognitive Processing Therapy (CPT)
CPT is a form of cognitive behavioral therapy that’s targeted at shifting the negative beliefs or "stuck points" that result from traumatic experiences using common CBT techniques.
It can involve an exposure component in the form of a written narrative or be conducted without an exposure component.
Medication
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs) are often prescribed to help manage PTSD symptoms.
Other medications, such as mood stabilizers, anti-anxiety medications, and sleep aids, may also be used depending on the individual’s needs.
Group Therapy
Group therapy and support groups, while not direct treatments for PTSD, allow individuals to connect with others who have experienced similar traumas.
Sharing experiences in a supportive environment can provide validation, reduce isolation, and promote healing by aiding in nervous system regulation.
It's important to note, that unlike other mental health conditions where medication is often viewed as a main treatment, psychotherapy is the primary treatment for PTSD with medications offering supplementary support. Treatment often involves trauma-focused psychotherapists and healthcare providers who can prescribe medication sharing health information and working together. Many healthcare professionals are able to recognize PTSD, but trauma-focused psychotherapists have dedicated themselves to providing specialized psychotherapy.
For a comparison and deeper dive into the main evidence-based treatments for PTSD, read our article, What is Typically the Best Treatment for PTSD?
Research-Backed Holistic Recovery Strategies
While trauma-focused psychotherapy is the gold standard for PTSD treatment, research within the six pillars of lifestyle medicine has shown there are practical evidence-based actions trauma survivors can take to support recovery and reduce PTSD symptoms. These lifestyle interventions can be grouped into the following pillars:
Nutrition
Following an anti-inflammatory diet can help restore the gut-brain microbiota, reduce inflammation, support brain health and has been shown to reduce PTSD symptoms in 9/11 survivors.
Movement
Multimodal exercise including aerobic, resistance training, and activities like yoga have shown to aid in the recovery process and help reduce PTSD symptoms.
Sleep
Sleep disturbance is often a warning sign for the development of PTSD and can maintain symptoms by interfering with memory processing and reducing emotion regulation. Taking actions to improve sleep can go a long way toward boosting recovery and helping therapy gain traction.
Stress Management
PTSD is a disorder of the stress response system but stress is an unavoidable aspect of life. Taking actions to reduce excessive stress levels and learning coping strategies to better manage unavoidable stressors is crucial for support PTSD recovery.
Social Support
Research consistently shows high benefit from multiple types of social support, particularly from frequent contact with supportive trusted friends. Developing a support system is a crucial aspect of recovery.
Toxin-Free Living
Self-medication and substance use disorder is highly prevalent in PTSD survivors, but substance use often exacerbates symptoms and can impede recovery. Reducing or stopping use either on your own or with the help of professionals is a crucial step to take for therapy to be effective.
To learn more about the research behind these lifestyle interventions and find tips on how to implement them, read our in depth series on The Six Pillars of Holistic Trauma Recovery.
Recovery Rates for PTSD
Recovery from PTSD varies widely depending on factors such as the severity of symptoms, the type of trauma experienced, co-occurring disorders, and access to treatment. With appropriate treatment, many people experience significant symptom reduction and an improved quality of life.
Natural Recovery Without Treatment
A large systematic review and meta-analysis including 81,642 participants estimated a spontaneous natural recovery rate of 44% within 40 months of initial diagnosis for individuals who did not receive treatment for PTSD.
Remission was defined as no longer meeting criteria for a PTSD diagnosis after at least 10 months.
The researchers noted that most natural remission occurs soon after diagnosis and is less likely as time passes, consistent with other research findings.
Research suggests that chronic long-term PTSD is less likely to remit on its own.
Impact of Trauma-Focused Psychotherapy
For those who do not experience natural remission from PTSD, or are unwilling to wait and see while experiencing unpleasant symptoms, trauma-focused therapy has shown to be more effective than no treatment at all, and more effective than general therapy or medications in many studies.
First-line therapies like EMDR are endorsed by highly authoritative organizations like the Department of Veterans Affairs for having large effect sizes on PTSD symptoms and achieving high levels of remission of PTSD by the end of treatment.
In a recent state of the science article on EMDR, the authors note that remission rates across studies range from 36% on the low end to 90% on the high end, and when follow-up measurements were taken the results were durable at 6 months and up to a year out post-treatment.
Long-Term Recovery
There is limited long-term research on the effectiveness of trauma-focused psychotherapy.
A recent meta-analysis on the short and long-term effects of trauma-focused psychotherapy found CPT and EMDR to have the strongest effects at 6-month follow-up post treatment.
The NICE Guidelines for the UK’s health system recommend EMDR for both it’s cost effectiveness (faster results) and durability at 1 and 4 month follow-ups.
Takeaway
While natural recovery is possible, as time passes it’s less likely, and up to 56% of people with PTSD may still have active symptoms after 3 years. Trauma-focused psychotherapy, particularly EMDR, is shown to be effective for reducing symptoms and achieving remission significantly better than no treatment or non-trauma-focused treatment. Although the research is limited, what’s available suggests that the effects of EMDR are durable at follow-ups.
It’s reasonable to conclude that combining trauma-focused therapy with holistic lifestyle changes and sustaining them after treatment supports long-term recovery. Though more research is needed to show the trajectory over the years, my experience in practice shows me most people experience meaningful improvement with therapy.
Conclusion
PTSD is a complex and challenging condition, but recovery is possible with the right combination of evidence-based treatments and support. Understanding the symptoms, diagnostic criteria, prevalence, and effective PTSD treatments can empower individuals to seek the help they need and take steps toward healing and recovery. If you or a loved one is struggling with PTSD, reaching out for therapy can be a crucial first step on the path to recovery. I would be honored to assist you on the journey to healing. If you’re interested in learning more about starting Eye Movement Desensitization and Reprocessing (EMDR) in Austin, TX, schedule a free 15-minute consultation to see if EMDR may be right for you.
Alex Penrod, MS, LPC, LCDC
EMDR Therapist | Founder | Neuro Nuance Therapy and EMDR, PLLC
Austin, TX
Last Updated: October 19, 2025
Disclaimer: This page is meant for educational purposes only and should not be taken as medical or clinical advice for the diagnosis or treatment of any medical condition. Consult with a licensed mental health professional for personalized guidance.
Frequently Asked Questions
-
PTSD is a trauma-related mental health condition that can develop after experiencing or witnessing a life-threatening or overwhelming event. It involves persistent distressing memories, avoidance, negative mood changes, and heightened nervous-system arousal lasting longer than 30 days.
-
While acute stress reactions are short-term, PTSD symptoms persist beyond one month and cause significant impairment. When stress responses occur after less severe, non-life-threatening events, they may be diagnosed as adjustment disorders instead of PTSD.
-
Symptoms fall into four categories: intrusion (flashbacks, nightmares), avoidance (avoiding reminders or feelings), negative changes in mood or cognition (guilt, shame, fear, hopelessness), and hyperarousal or reactivity (irritability, sleep problems, feeling constantly “on edge”).
-
Anyone exposed to trauma can develop PTSD, but risk is higher among those in high risk professions, with repeated or interpersonal trauma, limited social support, pre-existing mental health conditions, or a family history of mental health conditions. Protective factors include social connection, coping skills, and access to trauma-informed care.
-
A licensed mental-health professional assesses trauma exposure, symptom clusters, duration, and functional impact using DSM-5-TR criteria. A formal diagnosis requires the symptoms to persist for at least 30 days and significantly affect daily functioning.
-
Evidence-based therapies such as Eye Movement Desensitization and Reprocessing (EMDR), Cognitive Processing Therapy (CPT), and Prolonged Exposure (PE) are considered first-line treatments. Medication can help with co-occurring symptoms, but psychotherapy remains the gold standard for long-term recovery.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
Arena, A. F., Gregory, M., Collins, D. A. J., Vilus, B., Bryant, R., Harvey, S. B., & Deady, M. (2025). Global PTSD prevalence among active first responders and trends over recent years: A systematic review and meta-analysis. Clinical Psychology Review, 120, 102622. https://doi.org/10.1016/j.cpr.2025.102622
Blackmore, R., Boyle, J. A., Fazel, M., Ranasinha, S., Gray, K. M., Fitzgerald, G., et al. (2020). The prevalence of mental illness in refugees and asylum seekers: A systematic review and meta-analysis. PLOS Medicine, 17(9), e1003337. https://doi.org/10.1371/journal.pmed.1003337
de Jongh, A., de Roos, C., & El-Leithy, S. (2024). State of the science: Eye movement desensitization and reprocessing (EMDR) therapy. Journal of Traumatic Stress, 37(2), 205–216. https://doi.org/10.1002/jts.23012
Dworkin, E. R., Jaffe, A. E., Bedard-Gilligan, M., & Fitzpatrick, S. (2023). PTSD in the year following sexual assault: A meta-analysis of prospective studies. Trauma, Violence & Abuse, 24(2), 497–514. https://doi.org/10.1177/15248380211032213
Fantahun, A., Mamaru, M., Medfu, T. G., Girum, N., Techilo, T., Setegn, F., Gidey, R., Derbie, B. T., Jemal, S., Fasil, T. L., Muluye, G. G., Anmut, B. D., & Nega, G. T. (2024). Prevalence of posttraumatic stress disorder and associated factors among displaced people in Africa: A systematic review and meta-analysis. Frontiers in Psychiatry, 15, 1336665. https://doi.org/10.3389/fpsyt.2024.1336665
Hoell, A., Kourmpeli, E., & Dressing, H. (2023). Work-related posttraumatic stress disorder in paramedics in comparison to data from the general population of working age: A systematic review and meta-analysis. Frontiers in Public Health, 11, 1151248. https://doi.org/10.3389/fpubh.2023.1151248
Mavranezouli I, Megnin-Viggars O, Grey N, Bhutani G, Leach J, Daly C, et al. (2020) Cost-effectiveness of psychological treatments for post-traumatic stress disorder in adults. PLoS ONE 15(4): e0232245. https://doi.org/10.1371/journal.pone.0232245
Morina, N., Wicherts, J. M., Lobbrecht, J., & Priebe, S. (2014). Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long-term outcome studies. Clinical Psychology Review, 34(3), 249–255. https://doi.org/10.1016/j.cpr.2014.03.002
National Institute of Mental Health. (n.d.). Post-traumatic stress disorder (PTSD) — statistics. U.S. Department of Health & Human Services. Retrieved October 19, 2025, from https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd
Obuobi-Donkor, G., Oluwasina, F., Nkire, N., & Agyapong, V. I. O. (2022). A scoping review on the prevalence and determinants of post-traumatic stress disorder among military personnel and firefighters: Implications for public policy and practice. International Journal of Environmental Research and Public Health, 19(3), 1565. https://doi.org/10.3390/ijerph19031565
U.S. Department of Veterans Affairs & U.S. Department of Defense. (2023). VA/DoD clinical practice guideline for the management of posttraumatic stress disorder – Provider summary [PDF]. https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPG-PTSD-Provider-Summary.pdf
U.S. Department of Veterans Affairs, National Center for PTSD. (n.d.). Eye movement desensitization and reprocessing (EMDR) therapy – Treatment essential facts. Retrieved October 19, 2025, from https://www.ptsd.va.gov/professional/treat/txessentials/emdr_pro.asp
U.S. Department of Veterans Affairs, National Center for PTSD. (n.d.). How common is PTSD in Veterans? Retrieved October 19, 2025, from https://www.ptsd.va.gov/understand/common/common_veterans.asp
Watkins, L. E., Sprang, K. R., & Rothbaum, B. O. (2018). Treating PTSD: A review of evidence-based psychotherapy interventions. Frontiers in Behavioral Neuroscience, 12, 258. https://doi.org/10.3389/fnbeh.2018.00258
Yunitri, N., Chu, H., Kang, X. L., Wiratama, B. S., Lee, T.-Y., Chang, L.-F., … Chou, K.-R. (2023). Comparative effectiveness of psychotherapies in adults with posttraumatic stress disorder: a network meta-analysis of randomised controlled trials. Psychological Medicine, 53(13), 6376–6388. https://doi.org/10.1017/S0033291722003737