Self-Medication and PTSD: Moving Toward Toxin-Free Living
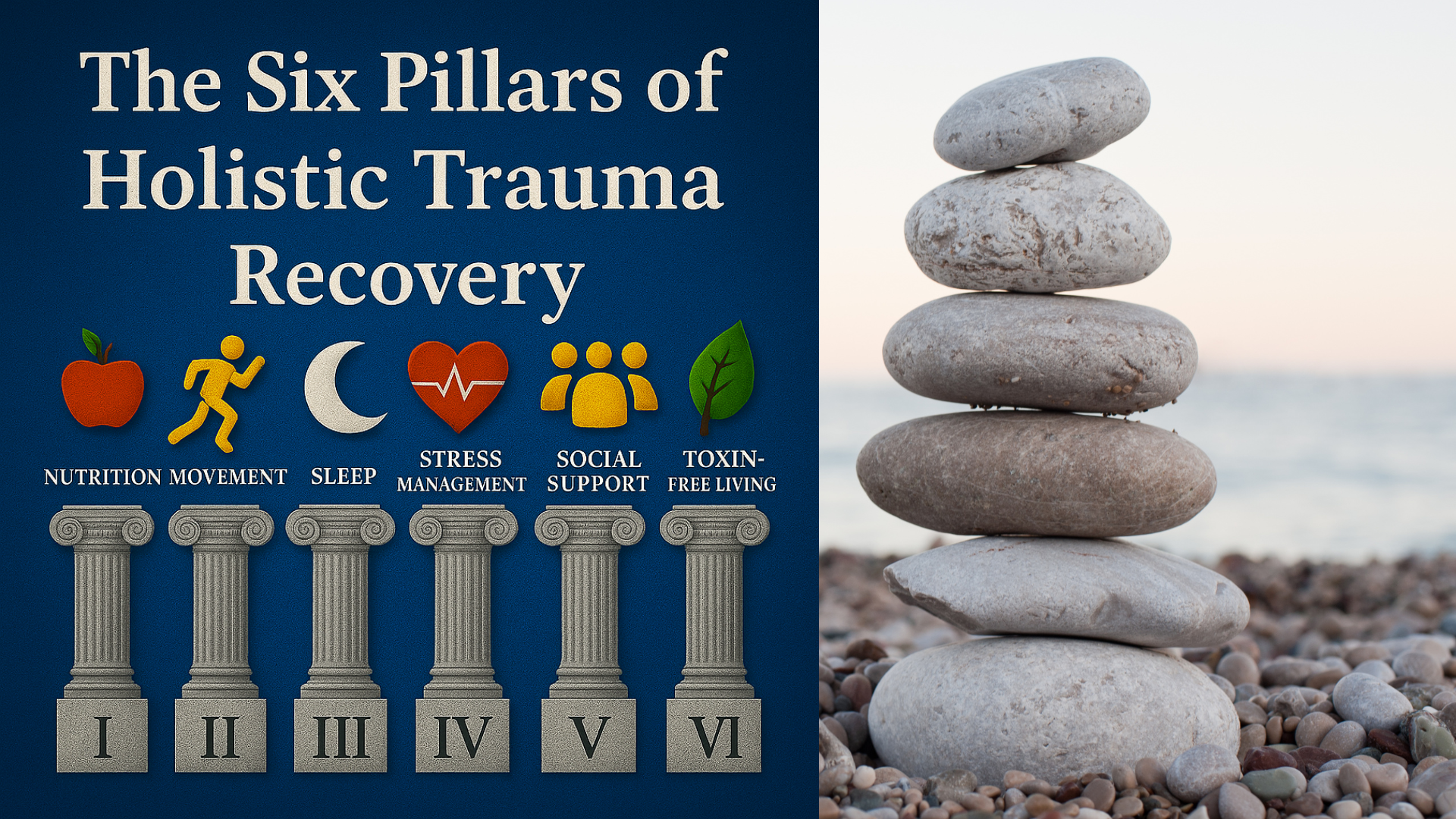
Pillar Six of a Six Pillar Approach to Holistic Trauma Recovery
Alex Penrod, MS, LPC, LCDC
EMDR Therapist | Austin, TX
Self-Medication and PTSD: How Trauma Survivors Can Heal Without Harmful Coping
Trauma changes how the brain and body experience safety. After a traumatic event, the nervous system can remain on high alert, flooded with stress hormones and intense emotional reactions that seem impossible to regulate. In that state, many people reach for something, anything, that quiets the noise. For trauma survivors, this often becomes the cycle of self-medication.
At first, drinking, using drugs, or even staying constantly busy can bring a sense of control or relief. But over time, those short-term escapes deepen the very symptoms of PTSD they were meant to soothe. Stable recovery requires more than stopping a behavior, it means understanding what the behavior was protecting you from and learning new ways to meet those needs.
This article is Pillar Six of a six part series, The Six Pillars of Holistic Trauma Recovery. It's also a topic that's near and dear to my heart as a person in recovery, an EMDR therapist, and a Licensed Chemical Dependency Counselor. My career began working in addiction treatment centers supporting people as they made one of the most difficult changes in their life.
Trauma recovery often looks like letting go of something that numbs the pain, creating enough safety and space to heal the wounds, and learning to adapt to life in ways that allow you to thrive rather than keeping you stuck. I've been honored to be a part of many such stories spanning the range of miraculous, tragic, and slow but steady progress. This article aims to offer you insight, resources, and hope.
Table of Contents
Understanding Self-Medication and PTSD
The self-medication hypothesis suggests that people use substances or behaviors to manage intolerable emotions or physiological states. For trauma survivors, that often means numbing intrusive memories, nightmares, or the constant sense of threat that lingers long after the danger has passed.
More than forty percent of individuals with a substance-use disorder also meet criteria for PTSD. This overlap, called comorbid PTSD, is common among military veterans, sexual-assault survivors, and those with histories of childhood trauma. Both conditions reinforce each other: substance use may dull flashbacks or negative emotions, but over time it worsens anxiety, depression, and leads to addictive disorders.
“It’s estimated that between 45–75% of people with a diagnosis of PTSD also meet criteria for a substance use disorder (SUD). Although trauma may provide the original catalyst for self-medicating, substance use and addiction become an independent problem on their own requiring specialized treatment in many cases. SUD also causes changes to the brain’s stress responses, making people more vulnerable to developing PTSD in the midst of an addiction. For successful recovery, both conditions should be addressed simultaneously by the right professionals.”
— Alex Penrod, MS, LPC, LCDC
Epidemiology and Risk Factors
Studies from the Department of Veterans Affairs and the National Comorbidity Survey show a high prevalence of substance use following trauma exposure, especially among combat veterans and war veterans who experience anxiety disorders or depressive symptoms after deployment. Rates of alcohol dependence and drug use disorders in these populations far exceed those in the general population.
The National Epidemiologic Survey on Alcohol and Related Conditions reports that people who self-medicate trauma symptoms have significantly higher odds ratios for developing alcohol use disorder, drug dependence, and chronic mental health conditions. Major risk factors include early exposure to violence, childhood trauma, limited social support, and untreated psychiatric disorders involving panic or generalized anxiety.
Why Self-Medication Feels Like It Works
In the moment, numbing feels like safety. Alcohol slows a racing heart; cannabis blunts intrusive thoughts; busy routines suppress memories. These coping mechanisms deliver temporary relief, a quick drop in emotional intensity that the brain mistakes for healing. But each episode of avoidance reinforces the belief that safety exists only through escape.
Over time, the brain’s reward circuits adapt. Dopamine spikes from substance use create craving, while the body’s stress systems remain hyperactive. Sleep, mood, and motivation begin to erode. Alcohol misuse and illicit drugs impair serotonin and GABA pathways, creating rebound anxiety when sober. What begins as a form of control slowly becomes another source of chaos.
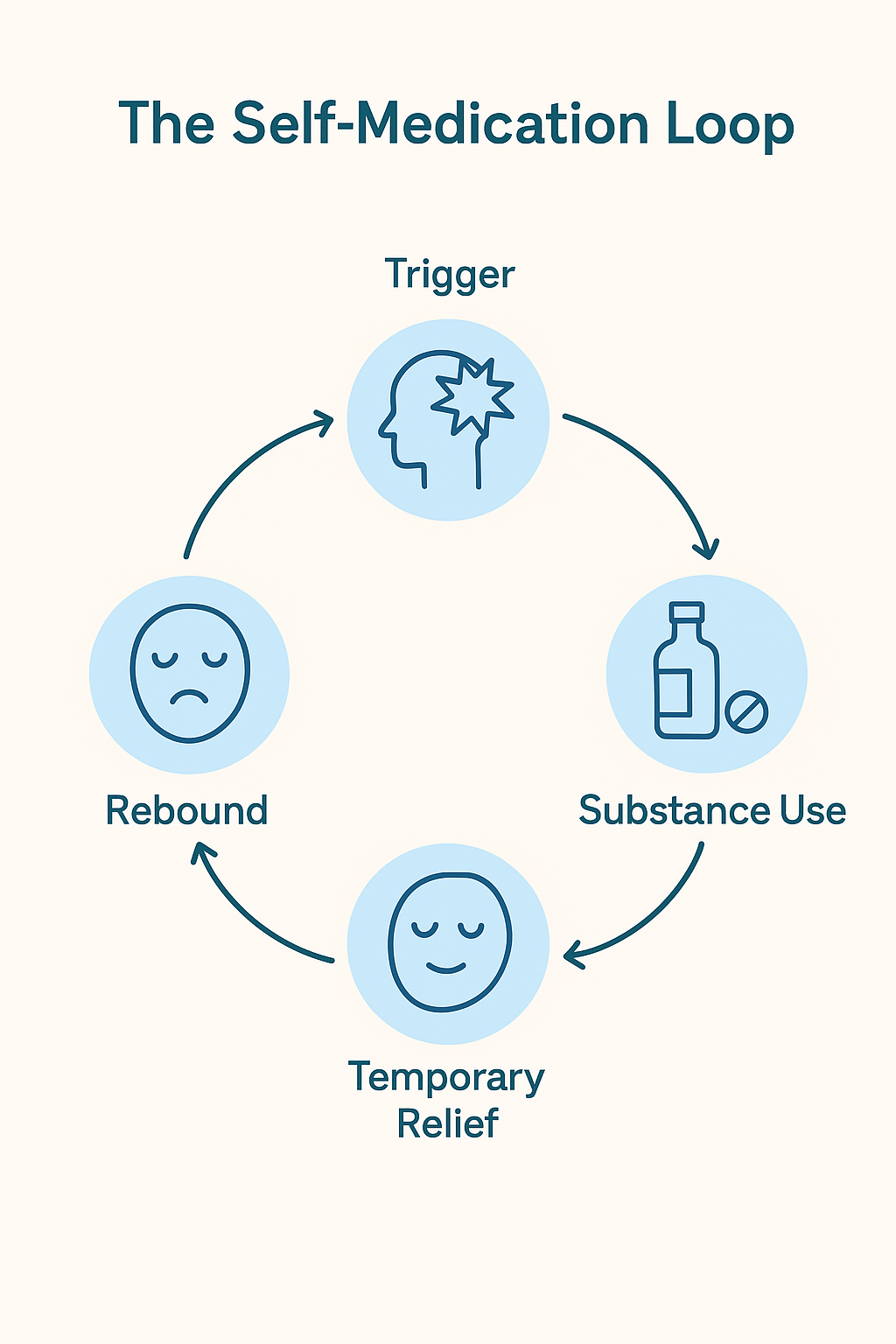
The Self-Medication Loop
Trigger
This could be a PTSD symptom, a response to the environment, or the dysregulating effects of substances themselves.
Substance Use
The response, reinforced by habit and neurobiology, becomes to ingest a substance to treat the unpleasant experience.
Temporary Relief
Relief is immediate, further reinforcing the coping mechanism, but temporary. Intoxication then prevents healing and the development of long-term coping skills.
Rebound
Intoxication suppresses certain functions of the brain, and the brain resists this by amplifying the function as the effects of the substance wear off. Alcohol will quickly reduce anxiety, but anxiety will return even stronger later, prompting more use.
How Self-Medication Worsens PTSD Symptoms
Substances that seem to help PTSD symptoms actually disrupt the very systems that support recovery.
Sleep disruption: Alcohol suppresses REM, the stage where emotional memories are processed and integrated. Without restorative sleep, trauma memories remain raw and intrusive.
Nervous-system dysregulation: Chronic intoxication prevents the body from practicing self-calming. Stress hormones remain elevated, and emotional reactivity increases when sober.
Cognitive impairment: The prefrontal cortex, which governs impulse control and perspective, becomes weakened, while the amygdala, responsible for detecting threat and triggering the stress response, becomes overactive.
Overlapping brain regions: the neurobiology of PTSD and addiction dysregulate the same brain regions, creating a loop of reinforcement by worsening symptoms, strengthening the compulsion to use for relief, and weakening the ability to resist the urge to use.
The Gut–Brain Connection
One of the most overlooked consequences of chronic substance use is its disruption of the gut–brain microbiota, the communication network between the digestive system and the central nervous system. This axis regulates inflammation, neurotransmitter production, and emotional processing.
Substance use reduces microbial diversity and increases intestinal permeability, leading to systemic inflammation and altered stress signaling. These changes amplify anxiety and irritability, core symptoms of PTSD, and can worsen alcohol addiction or drug abuse.
Chronic alcohol or drug exposure also impairs production of serotonin, GABA, and short-chain fatty acids, the chemicals essential for emotion regulation and neuroplasticity. This biochemical imbalance can blunt the effectiveness of trauma therapies like EMDR that rely on neural flexibility and emotional learning.
Is Cannabis Use Safe or Effective for PTSD?
While cannabis is a different class of substance than alcohol, stimulants, or opioid narcotics, it’s not without its risks, the effects appear temporary, and it doesn’t appear to help resolve the impact of traumatic memories. Although medical cannabis is prescribed for PTSD in some jurisdictions, authoritative sources such as the Department of Veterans Affairs report a lack of high quality evidence supporting cannabis for treating PTSD and they recommend against it. The majority of evidence for cannabis is anecdotal and based on short-term symptom relief while under the influence. Some research shows long-term worsening of symptoms.
The National Center for PTSD reports that although cannabis may not have the same harmful neurobiological effects as other substances, it has the potential to disrupt sleep stages, tolerance and dependence can develop, and there are functional impacts that often interfere with quality of life. Adherence to evidence-based therapies for PTSD may also be impacted. One study showed cannabis use predicted double the drop out rate in clients engaged in treatment for PTSD.
In summary, while cannabis may not be as harmful when compared to substances that severely dysregulate the brain and stress response, it doesn’t appear harmless and the reported benefits don’t appear to go beyond the benefits of any temporary avoidance or numbing strategy. For many who don’t have access to treatment, cannabis may offer a less risky and understandable method of self-medication. There are few effective pharmaceutical options for PTSD and therapy can be costly, time-intensive, and uncomfortable. It’s no mystery why so many people find their own solutions.
“From my point of view, this is not about moral judgment of whether substance use is right or wrong, it’s about whether a strategy actually treats the underlying condition for long-term relief or simply masks it temporarily. I believe people should be in charge of their own medical decisions while having access to the best information to make a decision. In the case of cannabis for PTSD, further research is needed.”
—Alex Penrod, MS, LPC, LCDC
Evidence-Based Treatment and Recovery
Healing requires compassion and structure. The Department of Veterans Affairs identifies evidence-based treatments such as Eye Movement Desensitization (EMDR), Prolonged Exposure Therapy, and Cognitive Behavioral Therapy as first-line interventions for PTSD.
Integrated Treatment Options
Because self-medication often leads to comorbid PTSD and substance use disorders, treatment must address both simultaneously. An individualized treatment plan may include:
Addiction treatment combining trauma therapy and behavioral health support at the appropriate level of care. This often involves the use of medication for detoxification, reducing craving, or stabilizing opioid use disorder.
Exposure therapy or EMDR for trauma processing once stabilization is achieved.
Coping skills training to replace avoidance with self-regulation strategies.
Group therapy or peer programs that rebuild connection and trust. Most people immediately think of AA, but there are multiple options for peer support.
Nutritional and lifestyle support to restore the gut–brain axis and improve quality of life.
Addiction and the Brain
Research on psychoactive drugs and neural reward pathways shows that repeated use alters dopamine signaling, making abstinence difficult without professional help. Integrated treatment helps re-train these circuits through consistent sobriety or reduced use, emotional regulation strategies, building new reward structures, and supportive relationships.
At Neuro Nuance Therapy and EMDR, PLLC, we use EMDR supported by Internal Family Systems, and ego-state therapy to heal traumatic memories and reorient the protective parts of the psyche that turned to substances for survival. Working with a trauma-specialist with dual certification in addiction recovery offers a natural next step when the healing process begins with addiction treatment.
Internal Family Systems and Parts Work for Self-Medicating
The IFS model conceptualizes the psyche as containing parts that adapted to living in the aftermath in trauma:
Managers — who proactively try to avoid being triggered by memories, reminders, or unpleasant states. These parts may self-medicate ahead of time.
Firefighters — who respond to emotional crisis after a triggering event has occurred. These parts may self-medicate to put out the flames.
Exiles — who carry the raw unprocessed memories of trauma. These parts are avoided and suppressed which prevents their healing.
The path out of self-medication involves gaining the trust of protectors, establishing a safe container for working with exiles and healing their pain, and reorienting protector parts to serving new functions that lead to long-term well-being vs short-term relief.
When Professional Support Is Needed
If you experience withdrawal, have a history of suicide attempts, or find it difficult to cut back despite consequences, specialized help is essential. Stopping the prolonged use of some substances, like alcohol and benzodiazepines, can be life-threatening, so medical treatment is crucial in these cases. Dual-diagnosis treatment centers and trauma-informed clinicians can address both trauma and addiction together, which is a critical factor in lasting treatment outcomes.
Many clients first enter therapy at the urging of a loved one or family members who see the toll of self-medication. Reaching out isn’t failure, it’s the first step toward balance. I know from experience that it never feels like the right time to seek help, but it’s something you don’t regret once the fog clears and the benefits of sobriety begin to materialize. For local resources in the Austin area visit our local resource article, Healing Trauma the Austin Way: How Holistic Living Supports EMDR Therapy.
How EMDR Therapy Supports Long-Term Recovery
EMDR therapy helps the brain safely revisit traumatic memories without overwhelm. Once self-medication behaviors lessen, neuroplasticity improves, allowing deeper integration of traumatic experiences and reduction of PTSD symptoms. EMDR has been found to lower cravings for substances when used to target cravings in special protocols, and also shows benefits above and beyond addiction treatment as usual when used to treat PTSD during addiction treatment.
Findings from systematic reviews of EMDR and trauma-related psychiatric disorders show consistent improvements in both PTSD and depression symptoms. Future research continues to explore how EMDR impacts long-term recovery rates after addiction treatment. IFS can be integrated with EMDR to help address compulsive urges to self-medicate and create stability for memory reprocessing.
Creating a Toxin-Free Path to Healing
Becoming “toxin-free” means clearing the layers of what keeps the body and mind dysregulated: substances, environments, relationships, and self-perception.
Reduce chemical exposure: Work with professionals to safely taper or stop alcohol and drugs.
Simplify your environment: Limit chaos and unpredictability. Create as much structure and safety cues as possible.
Reevaluate relationships: Surround yourself with people who support regulation, create boundaries and healthy distance with those who promote re-traumatization or self-medication.
Build daily regulation practices: Sleep hygiene, exercise, nutrition, mindfulness, and community connection all enhance recovery.
Replace shame with curiosity: Each urge to escape points to an unmet need, understanding these needs and finding new ways to meet them is the key to sustainable recovery. No one makes a perfect transition out of compulsive behaviors, slips can be converted into data to learn from rather than evidence of failure. Developing self-compassion along with self-accountability is vital.
Each step clears the internal noise, allowing calm, connection, and vitality to re-emerge.
Conclusion
Self-medication is not a moral failing, it’s a survival response that outlasted its purpose. Healing from PTSD involves learning to face pain with presence rather than avoidance. By addressing both trauma and substance use through integrated, evidence-based care, survivors can rebuild safety from the inside out. At Neuro Nuance Therapy and EMDR, PLLC, we help people in Austin, TX and across Texas heal the underlying wounds of trauma so self-medication no longer feels like a means of survival. If you’re looking for an EMDR therapist with experience navigating the road of recovery, schedule a free-15 minute consultation to learn more.
Reaching out can be difficult, but taking that step today can start your healing.
Alex Penrod, MS, LPC, LCDC
EMDR Therapist | Austin, TX
Disclaimer: This article is meant for educational purposes only. It is not intended to diagnose or treat any condition and should not be taken as medical or clinical advice. Seek the assistance of a medical or clinical professional for more personalized information.
Last Updated October 7, 2025
Frequently Asked Questions
-
Self-medication refers to the use of alcohol, drugs, or other behaviors to manage difficult PTSD symptoms such as intrusive memories, anxiety, hypervigilance, or emotional numbness. These strategies may offer temporary relief but often reinforce avoidance and make symptoms harder to treat over time.
-
According to the self-medication hypothesis, people may use substances to regulate intense emotions or physical sensations that follow a traumatic experience. Alcohol can help with sleep or anxiety in the short term, while cannabis or sedatives may temporarily calm hyperarousal. Over time, however, this pattern can lead to dependence, tolerance, and emotional avoidance that may interfere with long-term recovery.
-
Substance use can disrupt sleep, alter emotional processing, and impair brain systems involved in stress regulation. It may also interfere with therapies like EMDR, which rely on healthy memory reconsolidation and REM sleep. Over time, substance use can make it harder to regulate emotions or fully benefit from trauma-focused treatment.
-
Some individuals report short-term relief of anxiety or insomnia with cannabis, but research remains limited and mixed. The U.S. Department of Veterans Affairs cautions that cannabis use may sometimes worsen PTSD symptoms, reduce therapy effectiveness, or lead to dependence. More controlled studies are needed before it can be considered a reliable treatment option.
-
Recovery involves learning new ways to regulate stress and emotion, such as grounding, mindfulness, movement, and developing safe connections with others. Working with a trauma-informed therapist can help identify triggers, build healthier coping skills, and reprocess the memories driving PTSD symptoms for lasting relief.
-
It may be time to seek help if you notice withdrawal symptoms, increasing use, or difficulty functioning without substances. A trauma-informed clinician or dual-diagnosis treatment program can help address both PTSD and substance use together, improving emotional stability, sleep, and overall quality of life. Abruptly stopping heavy use of substances like alcohol or benzodiazepines can be dangerous and should always be done with medical assistance.

Learn More About Holistic Trauma Recovery
References
Godman, H. (2024, September 9). REM sleep: What is it, why is it important, and how can you get more of it? Harvard Health Publishing. https://www.health.harvard.edu/staying-healthy/rem-sleep-what-is-it-why-is-it-important-and-how-can-you-get-more-of-it
Goldstein, R. B., Smith, S. M., Chou, S. P., Saha, T. D., Jung, J., Zhang, H., Pickering, R. P., Ruan, W. J., Huang, B., & Grant, B. F. (2016). The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Social Psychiatry and Psychiatric Epidemiology, 51(8), 1137–1148. https://doi.org/10.1007/s00127-016-1208-5
Hill, M., Loflin, M., Hicks, T., Browne, K., & Norman, S. D. (n.d.). Cannabis Use and PTSD Among Veterans. U.S. Department of Veterans Affairs, National Center for PTSD. Retrieved September 5, 2025, from https://www.ptsd.va.gov/professional/treat/cooccurring/marijuana_ptsd_vets.asp
IFS Institute. (n.d.). Internal Family Systems model outline. https://ifs-institute.com/resources/articles/internal-family-systems-model-outline
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. https://doi.org/10.3109/10673229709030550
Logsdon, E., Cornelius-White, J. H. D., & Kanamori, Y. (2023). The effectiveness of EMDR with individuals experiencing substance use disorder: A meta-analysis. Journal of EMDR Practice and Research, 17(1), 21–32. https://doi.org/10.1891/EMDR-2022-0046
Shin, L. M., & Liberzon, I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35(1), 169–191. https://doi.org/10.1038/npp.2009.83
Substance Abuse and Mental Health Services Administration. (2020). Substance use disorder treatment for people with co-occurring disorders (Treatment Improvement Protocol 42). https://library.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PEP20-02-01_004.pdf
Sugden, K. J., & Merlo, L. J. (2024). Using lifestyle interventions and the gut microbiota to improve PTSD symptoms. Frontiers in Neuroscience, 18, 1488841. https://doi.org/10.3389/fnins.2024.1488841
U.S. Department of Veterans Affairs, National Center for PTSD. (2024). Treatment of co-occurring PTSD and substance use disorder in VA. https://www.ptsd.va.gov/professional/treat/cooccurring/tx_sud_va.asp
U.S. Department of Veterans Affairs & U.S. Department of Defense. (2023). VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder: Quick reference guide (Version 4.0). https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DOD-CPG-PTSD-Quick-Reference-Guide.pdf
Volkow, N. D., Michaelides, M., & Baler, R. D. (2019). The neuroscience of drug reward and addiction. Physiological Reviews, 99(4), 2115–2140. https://doi.org/10.1152/physrev.00014.2018
Whitworth, S. R., & Ciccolo, J. T. (2025). Lifestyle medicine and PTSD recovery. Frontiers in Psychology, 16, 11592247. https://pmc.ncbi.nlm.nih.gov/articles/PMC11592247/