Nutrition for Trauma Recovery: Pillar One of a Six Pillar Approach
Alex Penrod, MS, LPC, LCDC
Founder & EMDR Therapist | Austin, TX
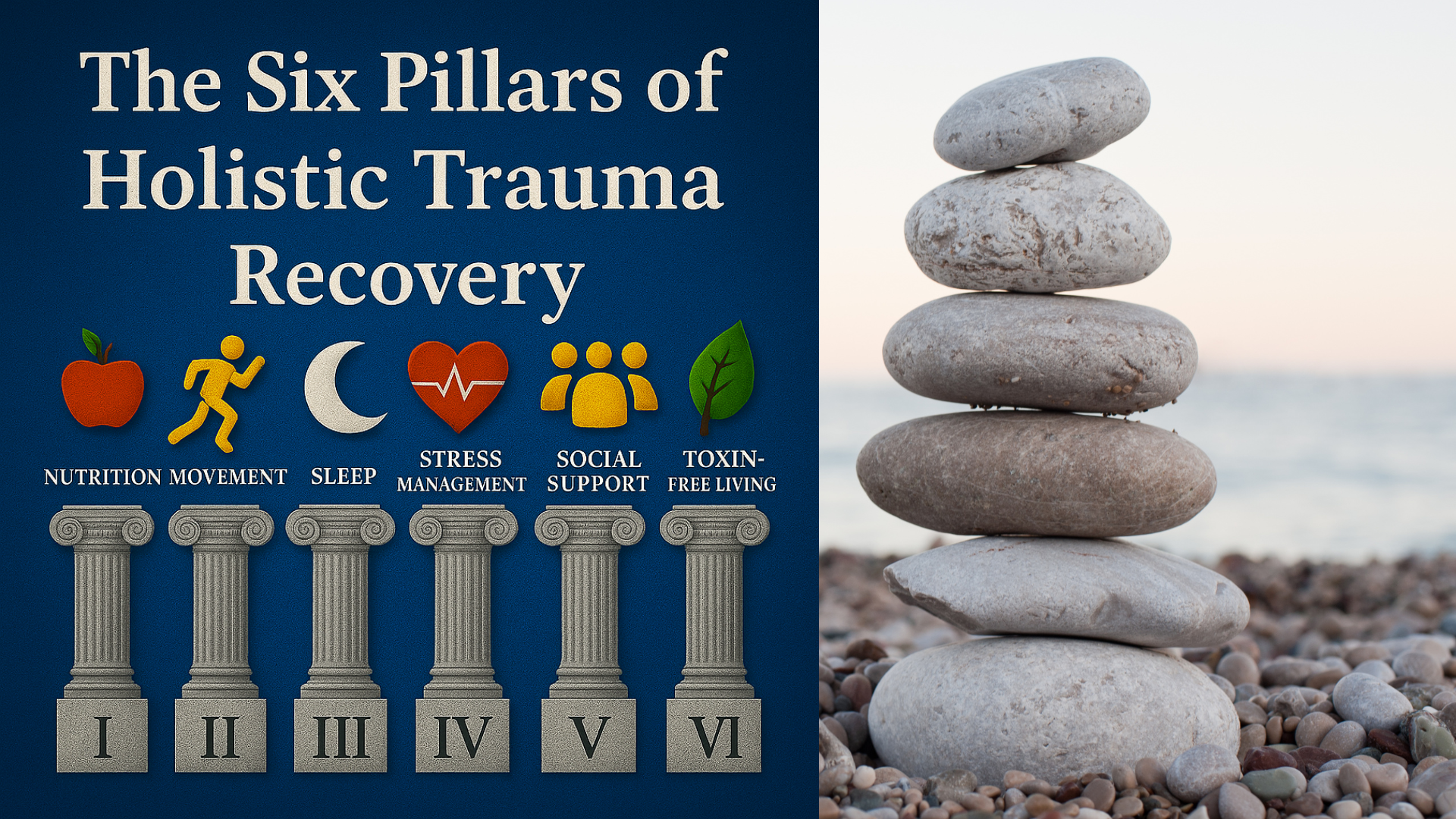
When we think of trauma recovery, therapy, yoga, EMDR, or medication may come to mind first. But research is increasingly showing that nutrition plays a crucial role in supporting the nervous system, reducing symptoms of trauma, and improving long-term outcomes for trauma survivors. From the gut-brain axis to the immune system to emotional eating patterns, our food choices profoundly impact the healing process. Nutrition is Pillar One in the Six Pillars of Holistic Trauma Recovery, and this article is the first of a six part series diving into each pillar.
Before we dive in, I'd like to give some background. As a trauma therapist, specializing in EMDR therapy in Austin, TX, I've always wanted a good framework to empower my clients to take charge of their healing process outside of therapy. So when I came across Sugden and Merlo's (2024) article, Using Lifestyle Interventions and the Gut Microbiota to Improve PTSD Symptoms, I knew I'd stuck gold. The Six Pillars of Lifestyle Medicine and Psychiatry have been around for a while, but when applied to trauma recovery they offer a powerful framework for organizing self-care and holistic strategies. I'm thrilled to share them with you.
Table of Contents
How Does Trauma Affect Eating Habits and Nutritional Status?
After traumatic experiences, it's common for people to experience shifts in appetite and eating habits. Some trauma survivors may under-eat, skip meals, or lose their appetite entirely. Others may overeat or turn to rich foods and sugar-heavy snacks as a coping mechanism. Emotional eating, body image concerns, and eating disorders are all common responses to adverse childhood experiences and chronic stress.
These patterns can lead to imbalanced blood sugar levels, nutritional deficiencies, and disrupted gut health, further complicating symptoms of Post-Traumatic Stress Disorder (PTSD) and other mental health conditions.
What is The Gut-Brain Axis?
The gut-brain axis is a bidirectional communication system that links our gastrointestinal tract with brain function. The gut microbiome, the community of microorganisms living in the digestive tract, influences inflammation, immune system activity, and neurotransmitter production.
What is the Role of Nutrition in Trauma Recovery?
Trauma often triggers a prolonged inflammatory response and oxidative stress, disrupting the gut microbiome and impairing the body's ability to regulate mood and stress. This is especially relevant for trauma survivors, whose nervous systems may remain dysregulated long after the initial threat is gone. Supporting gut health through proper nutrition is essential to improving overall health and managing symptoms of trauma.
Which Nutrients Support Trauma Recovery?
Eating a balanced diet rich in whole foods can help regulate the nervous system and support emotional well-being. Diets high in sugar and low in fiber tend to promote inflammation, while anti-inflammatory diets like the Mediterranean Diet have shown promise in reducing PTSD symptoms.
Key nutrients and foods that can support trauma recovery include:
Omega-3 fatty acids for brain health and inflammation reduction
Healthy sources of fat like extra virgin oil
Lean meats such as fish and chicken while limiting red meat
Leafy greens, whole grains, and fiber-rich foods to stabilize blood sugar and promote microbial diversity
Nutrient-dense foods are essential for trauma survivors dealing with mental health issues, as poor nutritional status can worsen symptoms and slow the healing process. Learn more about the Mediterranean Diet.
Can Nutritional Support Help with PTSD, Anxiety, and Depression?
Emerging evidence in clinical nutrition and nutritional psychiatry points to the profound impact of diet on mental health conditions. Nutritional interventions that emphasize anti-inflammatory foods and essential nutrients may improve brain function, reduce emotional reactivity, and support trauma treatment when paired with therapy. For individuals who struggle significantly with their relationship with food, body image, or eating behaviors that place them at risk, nutritional support from medical professionals alongside therapy is essential.
Although nutritional supplements like high dose vitamins may be helpful in some cases, they should always be used under the guidance of healthcare providers as part of a multidisciplinary approach. Be wary of Instagram influencers who make fantastic claims or promote supplements that may actually be quite risky.
Randomized controlled trials suggest that dietary changes can reduce symptoms of PTSD and improve cognitive function within months. However, the most sustainable outcomes come from long-term shifts in eating habits and lifestyle rather than short-term fixes.
How can Nutrition be Integrated into the Healing Process?
As a therapist, I support my clients in becoming more aware of how their eating patterns relate to emotional states. I also share nutritional education and research to give my clients another avenue to take charge of their healing. A holistic approach to trauma recovery includes not only EMDR or talk therapy, but also attention to physical health, nutritional support, and stress reduction.
For my clients interested in improving their nutrition I recommend collaborating with dietitians, functional medicine providers, or integrative healthcare professionals. These experts can create trauma-informed nutrition plans that meet individual nutritional needs and address side effects of trauma-related disorders. The most effective approaches are guided by individual testing and examination prior to making any significant changes.
Getting Started: Small Steps Toward a Trauma-Informed Diet
Nutrition for trauma recovery doesn’t mean following a rigid plan. It can start with small, mindful changes:
Swapping ultra-processed foods for whole foods where possible
Including leafy greens, healthy fats, and fiber in daily meals
Staying hydrated and eating at regular intervals to support blood sugar balance
Avoiding restrictive diets that may worsen body image or emotional eating patterns, unless given specific direction from a medical professional.
By focusing on long-term, sustainable food choices, trauma survivors can begin to reclaim a sense of agency over their physical and emotional well-being.
Conclusion
Nutrition is not a cure for trauma, but it is a powerful ally. With proper nutrition, trauma survivors can support their nervous system, reduce inflammation, and improve outcomes of trauma treatment. Working with healthcare providers as part of a multidisciplinary approach can ensure that nutritional interventions are safe, supportive, and sustainable. This is especially important for those who find their relationship with food to be a major challenge. Best practices when eating concerns are at the forefront include working with a physician and dietician alongside a trauma therapist.
Whether you're researching for your personal interests, planning for, or actively engaged in a trauma recovery process, I want to empower you to keep taking the next step toward your goals.
Neuro Nuance Therapy and EMDR, PLLC | Austin, TX
Last Updated October 5, 2025
Disclaimer: This article is meant for educational purposes only. It is not intended to diagnose or treat any condition and should not be taken as medical or clinical advice. Seek the assistance of a medical or clinical professional for more personalized nutritional and dietary advice.
Frequently Asked Questions
-
A balanced, anti-inflammatory diet helps regulate your nervous system, stabilize blood sugar, and support the gut-brain axis, all of which are disrupted by trauma. Nourishing your body with whole foods gives your brain the nutrients it needs to process stress, improve sleep, and restore emotional balance.
-
Nutrients that calm inflammation and strengthen brain health include omega-3 fatty acids (salmon, chia, flax), antioxidants (berries, leafy greens), and complex carbohydrates (quinoa, oats, vegetables). These foods promote neurotransmitter balance and energy stability during trauma recovery.
-
Yes. Research in nutritional psychiatry shows that anti-inflammatory diets like the Mediterranean pattern can improve mood, resilience, and emotional regulation. Nutrition doesn’t replace therapy, but it complements trauma-focused treatments such as EMDR by supporting the body systems that make emotional healing possible.
-
The gut-brain axis is the communication network between your digestive system and your brain. Trauma and chronic stress can disrupt this connection, increasing inflammation and mood symptoms. Eating fiber-rich, whole foods supports a diverse microbiome that can help regulate stress hormones and emotional stability.
-
Some supplements like omega-3s, magnesium, or vitamin D may help, but they should always be used under professional guidance. Your nervous system heals best with consistent, real-food nourishment rather than high-dose or trend-driven supplements. Consult dieticians and functional medicine specialists before trusting Instagram.
-
Begin with one small, sustainable change, such as adding a daily serving of greens or drinking more water. Trauma recovery takes patience; consistent nourishment, not restriction, helps your system heal. Working with a trauma-informed therapist and dietitian can help you build a plan that supports your unique healing process.
-
No. Nutrition is one of the Six Pillars of Holistic Trauma Recovery. It strengthens your body between sessions, but it doesn’t replace trauma-focused therapy or prescribed care. Together, these approaches help restore balance to both body and mind.

Learn More About Holistic Trauma Recovery
References
Arcan, C., Hou, W., Hoffman, K., Reichardt, A., Yang, X., Clouston, S. A. P., Bromet, E. J., & Luft, B. (2023). Mediterranean diet intervention among World Trade Center responders with post-traumatic stress disorder: Feasibility and outcomes of a pilot randomized controlled trial. Obesity science & practice, 10(1), e725. https://doi.org/10.1002/osp4.725
Ke, S., Hartmann, J., Ressler, K. J., Liu, Y. Y., & Koenen, K. C. (2023). The emerging role of the gut microbiome in posttraumatic stress disorder. Brain, behavior, and immunity, 114, 360–370. https://doi.org/10.1016/j.bbi.2023.09.005
Merino Del Portillo, M., Clemente-Suárez, V. J., Ruisoto, P., Jimenez, M., Ramos-Campo, D. J., Beltran-Velasco, A. I., Martínez-Guardado, I., Rubio-Zarapuz, A., Navarro-Jiménez, E., & Tornero-Aguilera, J. F. (2024). Nutritional Modulation of the Gut-Brain Axis: A Comprehensive Review of Dietary Interventions in Depression and Anxiety Management. Metabolites, 14(10), 549. https://doi.org/10.3390/metabo14100549
Sugden, S. G., & Merlo, G. (2024). Using lifestyle interventions and the gut microbiota to improve PTSD symptoms. Frontiers in Neuroscience, 18, 1488841. https://doi.org/10.3389/fnins.2024.1488841
van den Berk-Clark, C., Secrest, S., Walls, J., Hallberg, E., Lustman, P. J., Schneider, F. D., & Scherrer, J. F. (2018). Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occurring smoking: A systematic review and meta-analysis. Health Psychology, 37(5), 407–416. https://doi.org/10.1037/hea0000593